Week 2: Interventions to prevent effects of extreme heat
Module 3 Week 2: Interventions to prevent effects of extreme heat
Welcome to the second week of the third module of this e-learning!
 This week you will focus on the different types of prevention, and on using it on a micro-level.
This week you will focus on the different types of prevention, and on using it on a micro-level.
This week’s work:
1. Before getting deeper into prevention and possible interventions, we will start off with the case of Mr. Johnson (See the Map ‘Cases’). Please read it, and formulate a first global advice to Mr Johnson. Later this week, we’ll get back to him.
2. Then, please check this video clip and learn about several practical things that can be done to prevent heat stress.
Which of these interventions, do you think, could be helpful for Mr Johnson? Write them down!
3. To understand the different types of prevention, please watch this short lecture and then read the text underneath.
Many of the interventions mentioned in the articles you have read, and the clips you have seen, can be considered as a form of prevention. Should you want to develop a preventive strategy, you need to have a good understanding of the different types and stages of prevention. Although there is no uniform, generally applicable definition of prevention, the WHO has adopted a description of prevention that has become generally accepted, especially in healthcare. Here, a distinction is made between primary, secondary and tertiary prevention. In this context, primary prevention refers to all measures that can be taken to prevent the occurrence of the basic problem. In this e-learning and depending on the perspective chosen, that could be the appearance of extreme heat or the occurrence of heat-induced problems in the elderly. Secondary prevention includes measures that can be taken in high-risk situations, for example in case a heat wave occurs, and the elderly have symptoms predicting related health problems. Tertiary prevention deals with the reaction of the elderly who actually suffer from heat-related health problems. This type of prevention is directed at reducing complications. In this classical prevention model, there is a clear timeline: no problem, or not yet any problem, (primary), small, beginning problems (secondary), and serious problems (tertiary).
Another and more recent ‘prevention model’ which has been introduced by the Institute Of Medicine (IOM) is widely employed lately. In this model it’s not the timeline, but the target groups that are distinctive: universal prevention which is directed at the overall population, selective prevention which is geared toward high-risk groups, and indicated prevention when individuals are facing (potential) health problems.
Both models (WHO and IOM) can be used separately, but also in combination since the distinctions made are related, which is illustrated in Figure 2.
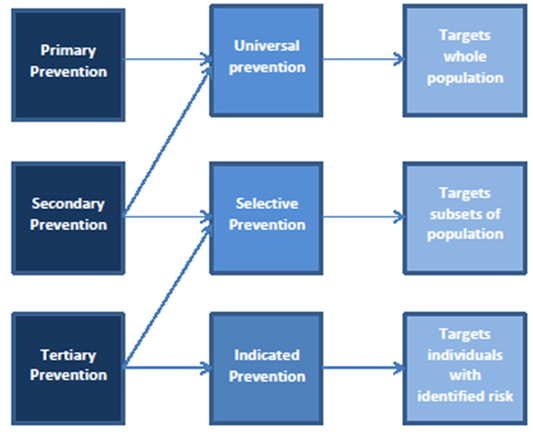
Fig 2. The relation between the WHO and IOM prevention model. (Meili B: Indizierte Prävention bei gefährdeten Jugendlichen. Suchtmagazin 2004, 6:21–25.)
Considering this, secondary prevention is not only important for individuals at high risk but also for the overall population. Furthermore, tertiary prevention should not only be considered similar to indicated prevention since it can be applied in high-risk groups too.
3. Now, could you write down 3 measures that can be considered as universal prevention, 3 as selective prevention, and 3 as indicated prevention?
4. After you have done this, please check again the main article (Ollie Jay et al. ) from the first week of this module. And answer the question of which of the (at least) 9 interventions you have mentioned, can be considered as proven effective according to autors.
Knowledge Check
To check whether or not you have understood most of the material: please read again the case of Mr Johnson. Please write down at least 5 preventive measures you can think of. On the dialogue cards below you wil find some tips that can help you with this task.
--------------